More than a decade ago, little was known about the myriad of microorganisms that live happily inside and on our bodies. Now researchers believe they could change the future of human health.
It was May 2012 when Amanda Kabage, a then 32-year-old paediatrics researcher at the University of Minnesota, started having unusual gastrointestinal problems. She suffered more than ten bowel movements a day and would find worrying amounts of blood in her stool. To doctors it looked like a minor bacterial infection, so she was prescribed a course of two different antibiotics.
Months went by, and the symptoms kept getting worse. She was a young, healthy, fit woman who was suddenly having chronic abdominal pain, forcing her to give up solid foods and losing 20lbs (9kg). Her hair fell out in clumps and her absences from work began to be noticed by colleagues. She was prescribed several medications to no avail.
In November that year, she was eventually diagnosed with a bacterial infection known as Clostridium difficile, or C. diff for short. Although this bacterium can be found in the guts of most people, if it grows out of control it can release toxins that damage the intestines and kill other bacteria that keep the organ functioning. The infection often arises as a result of taking strong antibiotics, which upset the gut's healthy ecosystem.
It is a common problem, causing millions of infections and thousands of deaths around the world every year. One recent review estimated the global burden of C. difficile is around 323 cases for every 100,000 people, or about 25 million cases globally.
But since no treatment was alleviating her pain, Kabage put her research skills into practice. She trawled through scientific papers and, not without pushback from her doctors, personally reached out to a leading C. difficile researcher to ask if she could take part in a trial of an experimental therapy they were working on that involved transplanting the gut microbes from a healthy person into patients.
In early September 2013, Kabage underwent the procedure, known as a faecal microbiota transplantation, or FMT. Donor stool with a healthy concoction of microbes was transplanted into her gut to replace her damaged microbiota.
"That night, there was all this rumbling going on in my guts, like my new microbes were finding their new home and establishing themselves in my colon," Kabage says. The effect was rapid and astounding. After 14 months of suffering, two weeks after her treatment Kabage was back to her normal self. The gastrointestinal issues had fully disappeared.
The treatment she received is the culmination of a growing realisation that microorganisms that make their homes inside our bodies play an important, if somewhat underappreciated role in our health. Scientific research has helped to uncover the complex interactions between our general wellbeing and the flora flourishing on and in our mouths, noses, airways, lungs, stomachs, colons, sexual organs and skin. They help us digest, metabolise, produce mucus, lubricate and form a first line of defence against foreign organisms that might harm us.
As our understanding of this complex and life-long relationship unfolds, so does our ability to harness it to our benefit. It is leading many experts to hope that we may soon be on the cusp of a new era of healthcare that nurtures and tweaks our microbial hitchhikers for our own benefit.
The microbiome era
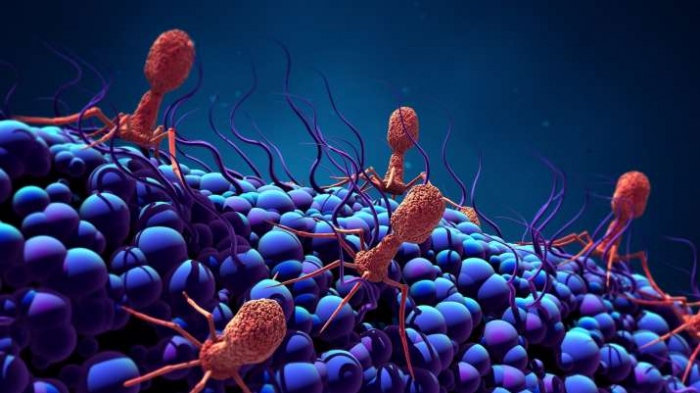
It is best to think of the microbiome as a city of communities. It is composed of trillions of bacteria, fungi, and virus neighbours, all jostling for space inside and on the surface of our bodies. As they live out their existence in their own neighbourhoods, they also perform roles that benefit the wider body. A healthy microbiota is a bountiful, diverse one, and everything from our diet to our environment affects how well it functions.
But the overuse of antibiotics and consumption of ultra-processed foods, for example, are decimating our gut microbiota, leaving people more vulnerable to infections like C. difficile and other forms of disease. Exactly how significant this relationship between our microbiomes and our health is only now becoming clear.
Perhaps the most significant step has been the realisation that we can also use our microbiota to help us treat or even prevent disease. The emergence of hypervirulent strains of C. difficile have led to a huge increase in cases in the past 20 years and over 20% cases now involve bacteria that have become antibiotic resistant. It has meant our standard approach for fighting these infections – with a course of antibiotics – is becoming increasingly useless. Those that do work are used sparingly for fear of triggering resistance to them too.
But FMT has offered an alternative in the battle against infections such as C. difficile. By effectively restocking a healthy balance of microbes in the gut, it allows those bacteria to bring numbers of C. difficile back under control.
"You can say this past decade was the decade of emergence of FMT into clinical practice," says Alexander Khoruts, medical director of the University of Minnesota's Microbiota Therapeutics Program, and a pioneer in the FMT field. "Now we're entering a new chapter that is a bit more serious in terms of product development. This [FMT] essentially was just a chapter in what's probably going to be a story that will just continue this whole frontier of medical therapeutics."
Ancient origins
The use of faecal matter in medical treatments can be traced back to the ancient Egyptians, who used human and animal stools as active ingredients against a variety of ailments. But as modern medicine led doctors to appreciate the need for hygiene to maintain aseptic environments, the use of faeces fell out of use. They didn't make a comeback until 1958, when a Colorado researcher re-ignited interest in FMT treatment among his colleagues.
"It was mentioned when I was going to medical school in the 1980s, and the students kind of giggled," says Khoruts. It wasn't until 2008 that Khoruts was able to carry out his first FMT, which helped to establish procedures for sampling the donor and recipient microbial community before and after the treatment. He was able to show that the transplanted bacteria stayed in the donors' guts for over a month.
DIY treatments can sometimes be risky because there's no way of knowing what lives in the donor's guts
His laboratory then developed a protocol for freezing stool mixtures for long-term storage, so that doctors no longer had to prepare faeces slurries in their offices. Instead, they could rely on pre-prepared samples. Standardising the process paved the way for making FMT more widespread.
Patients can now receive FMT in the form of a colonoscopy, an enema, or oral ingestion through small capsules of frozen-faecal material.
It was Khoruts who treated Kabage in 2013. That year, after a regulatory tug of war between academics, business and international regulators, FMT was approved for treatment of C. difficile under very stringent rules, which vary from nation to nation in their definition of whether FMT is a transplant of tissues or an experimental biological drug. Ever since, it has been used to treat thousands of patients in Europe and the US each year (although exact numbers are hard to find). Researchers believe, however, that it has the potential to help many more.
Without easy access to these treatments, however, some people have taken matters into their own hands… quite literally.
In 2011, Carolyn Edelstein founded the microbiota organisation OpenBiome after her cousin gave himself an FMT on his own, in his bathroom, with faeces donated by his housemate. Such DIY treatments can sometimes be risky because there's no way of knowing what lives in the donor's guts, and if it matches the recipient's gut. The need for rigorous testing of donor microbiota was underlined after a rare form of drug-resistant E. coli was found to have been transferred to two patients, one of whom subsequently died, during a clinical trial at a hospital in the US. But despite this there are still several accounts of DIY treatments being a widespread trend.
What Edelstein's organisation created in response is "like a blood bank, but for stool", she says. In a laboratory in Cambridge, Massachusetts, scientists clad in poop-emoji-print lab coats prepare solutions of liquefied donor stools and store them in labelled vials in massive freezers. The advantage of having so many stool samples in one place is that, "we can be a lot more rigorous than you can be when you're doing a single donor per patient", says Edelstein.
On a large scale, they can thoroughly screen donor faeces for anything that might cause complications – donors are put through extensive medical interviews, blood tests, and then the faecal matter itself is tested for common gut pathogens like Salmonella and E.coli, parasites, viruses, and antibiotic resistant bacteria before they are stored ready for transplantation.
OpenBiome has since provided over 60,000 treatments to clinics and hospitals. But it is now looking beyond faeces transplants, as regulation continues to shift.
From poop to pills
Recently the Food and Drug Administration in the US raised safety concerns about faecal microbiota transplants after six patients who received faecal transplants from a stool bank suffered serious infections that resulted in them needing hospital treatment.
It is just one reason that has led scientists to look for alternative ways to harness the power of the microbiome.
OpenBiome, for their part, have launched a sister biotechnology company to continue research on the specific communities of microbes that can be used to restore a healthy functioning gut ecosystem.
"We always kind of knew that there would be this bridge period, and it was our goal to say that we care about helping patients who need it today, until there's a moment where the field is able to take that baton and provide those commercial alternatives," Edelstein says.
Although drugs that target the microbiome are still undergoing clinical trials and so are not yet available to the public, many researchers expect that by the end of 2022 over-the-counter treatments may be available. Rather than transferring faecal matter, however, these are more likely to be capsules of microbes extracted from the stools of healthy patients.
OpenBiome's sister company, Finch Therapeutics, is currently in the late-stage clinical development of a drug called CP101. The drug is basically a freeze-dried, intact microbiota community harvested from healthy human donors before being screened in a laboratory and then put in capsules. Another company, Rebiotix is doing something similar, with their new drug RBX2660, and so are a number of other firms including SERES, Vedanta, Siolta Therapeutics, and Servatus. One company, Axial Therapeutics, wants to use microbiota analysis to better understand the relationship between microbes and the central nervous system in the hope of creating new pharmaceuticals.
All of these companies are aiming to offer something more advanced, and perhaps more palatable to patients, than the current FMT solution.
"FMT was never intended to be a treatment," says Raja Dhir, who is on the board of directors for the Microbiome Therapeutics Innovation Group, a coalition of pharmaceutical and biotechnology companies working for regulatory approvals for microbiome therapeutics. Transplanting faecal matter from a donor was a crude tool to create a healthy ecosystem, according to Dhir, but the future will involve a more carefully selected set of microbes that are cultured in a controlled laboratory setting. The aim is to have more control over what's actually going into the patient's body.
"In many ways, microbe-based therapies go through the same process as any therapy looking for FDA approval," says Dhir. He also is the founder of Seed, one of a number of microbial health companies pioneering the field: "I think we will improve the efficacy of many existing treatments like cancer therapy by considering the gut microbiome in the future." However, the role that the gut microbiome might play in cancer management is still being investigated by researchers.
But treating patients through their microbiome is not likely to be as straight-forward as giving everyone a pill to pop. While 99.9% of a person's genome looks like anyone else's, only 10-20% of the microbes in your gut will be shared by someone else. The species and variants of microbes found in our bodies can vary wildly. The human genome consists of just 23,000 genes, while the microbiome as a whole contains many millions.
Personalising treatments when there is this much variety is a Herculean task, and a lot of research still needs to be done.
Some companies, however, claim to offer behavioural coaching from dieticians based on analysis of a patient's microbiome using AI while another is attempting to decode the microbiomes of super-performers such as Olympic athletes in the hope of finding nutritional solutions that might assist optimal physiology.
"There's just so much complexity to the interactions of these microbes and how they work," says Edelstein. "It can be difficult to predict what happens when you're isolating a particular species from that complex ecology and trying to introduce it into a very different environment in a new host."
What's a healthy microbiome?
In order to advance therapeutics, scientists need to answer some existential questions: what is a healthy microbiome in the first place and how does lifestyle affect it?
The Global Microbiome Conservancy (GMC) is an organisation that searches for unique microbes which are being wiped out by excessive antibiotics use, or eating processed foods. It is hoping to catalogue these by collecting samples of populations living in remote areas who are not exposed to these harmful aspects of life in industrialised societies. To date most research on the microbiome has been done in wealthy, Western nations.
"By focusing most of our research on the urban microbiome of people living in industrialised countries, we are not only missing the full scope of microbiome diversities, we also look at microbiomes that are not necessarily representative of what healthy microbiomes should be," says Mathilde Poyet, co-founder of GMC. Gut microbiomes of peoples living in urban centres of industrialised countries lack numerous key bacteria and functions, she says.
Each month, her team travels around the world with a "portative lab" to take faecal microbiome samples from remote communities. For example, they collaborate with Muhammad Imran, a professor of microbiology at Quaid-i-Azam University Islamabad, to take samples from the Hunza population in northern Pakistan.
"We are trying to sample from a distinct population, so that we can conserve these microbiota that have been part of the human gut over the centuries and which we are actually losing because of our own practices, like consuming a lot of antimicrobial agents from our foods," Imran says.
"Nutritional habits here in Pakistan and largely the subcontinent are quite different from Europe and US," Imran adds, mentioning, for example, their extensive use of spices and fermented foods. According to Imran, fermented foods, specifically, encourage diverse microbial ecosystems because they are rich in live bacteria and yeasts.
Diet, in fact, is crucial to microbiome health.
"You can make big shifts in your microbiome by making shifts in your diet," says Tim Spector, a professor of genetic epidemiology at King's College London, in the UK. When he started his research, he had his son eat fast food at every meal for ten days straight to prove what damage it can cause the gut microbiome.
He has launched Zoe, a gut-health app where users provide a blood and faeces sample along with a food diary for scientists to analyse against data from a series of large scale studies quantifying how the body and its microbiome responds to different foods. The results are sent back as a personalised diet recommendations that aim at improving the user's microbiome.
You can make big shifts in your microbiome by making shifts in your diet – Tim Spector
Through this app, Spector is also conducting the world's largest nutritional research program, to finally answer questions about how diet affects the microbiome.
"We're still scratching the surface, but there has been great progress in some areas," Spector says. In the next decade or two, "it's going to be really understanding what those microbes do, what their function is, what chemicals they produce… we will be able to get a catalogue of different foods that are likely to affect these communities," he says.
The future of microbiome therapeutics
This new era of innovation in microbiome therapeutics could at least help patients depart from the ick factor tied to FMT, says Christian Lodberg Hvas, a clinical associate professor at Aarhus University in Denmark. "Swallowing faeces is quite controversial for most people," he says.
In the future, he thinks we might even reach a point where it will be possible to pick and choose microbes from a library of helpful bacteria to treat different diseases. "Targeted microbiota therapy – basically live biotherapeutics – is going to be rising. And then FMT will be placed somewhere in a corner," he says. "But we don't even know if we're focusing on the right things. We have high hopes in microbiota and some of the hopes are realistic and may be achieved, and a lot of the hopes are illusions."
Who knows what connections we may find, he says. Researchers in Finland are looking at how c-sections or natural births affect the microbiome.
Scientists are also looking into using microbiota transplants for a wide range of disorders, such as insomnia, Parkinson's disease, HIV, chronic fatigue, multiple sclerosis, obesity, insulin resistance, metabolic syndrome, and autism.
Among those conducting research into the links between the microbiome and C. difficile, irritable bowel syndrome, and autism, for example, is Amanda Kabage. Following her own experience with FMT in 2013, she joined Khoruts' Microbiota Therapeutics laboratory.
"I think this is going to be the thing that's going to impact most areas of medicine," she says when asked about what she thinks the future of microbiome therapy might hold. "I'm really excited to have the possibility that many more things out there could be potentially affected by just fixing our gut."
More about: