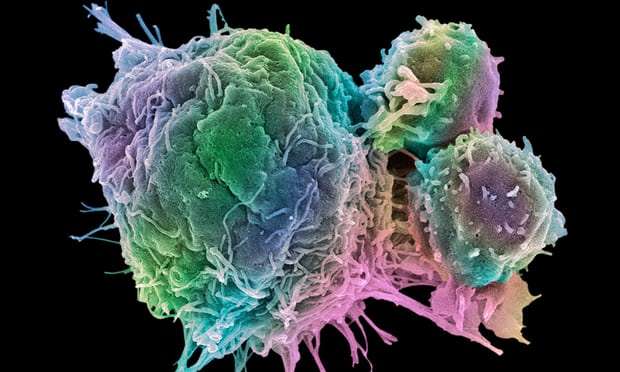
A groundbreaking international collaboration has shown how tumours in different parts of the body, which have previously been treated as separate diseases, have molecular similarities which could render them vulnerable to drugs already on the market.
The research redefines cancer types beyond terms such as breast and bowel, which are descriptions only of where the cancer first arose. Instead, the newly uncovered molecular makeup of cancers could lead to “drastic changes” in how the best drugs for patients are chosen.
Doctors told The Independent it could change the “traditional” method of treatment based on the location of tumours and allow clinical trials to “identify patients most likely to benefit” from experimental drugs.
The Cancer Genome Atlas is the largest project of its kind and contains the genetic information for every cell of tumours taken from more than 11,000 patients, across 33 different types of cancer.
Comparing this new data with information on treatments licensed for use in other cancers, the authors showed that 50 per cent of these 11,000 tumours were had potentially effective treatments already out there.
The project also traced these tumours back to mutations in 300 different genes, including well studied types like the BRCA 1 and BRCA 2 genes, where mutations significantly increase the risk of breast cancer.
It also found that around 8 per cent of the cancer-causing mutations were inherited from parental DNA, rather than mutations caused by things like sun damage or smoking.
The authors compare their work to the conclusion of the human genome project, which first transcribed every line of our DNA and introduced the prospect of medicine personalised to each person.
“In effect, biomedical science is now graduating from studying the tumour in isolation to assessing it within its larger environmental context. The findings described here suggest drastic changes in clinical practice and drug development,” they write in a summary.
While this work itself doesn’t immediately mean new cancer treatments, it can be built on by other teams in drug development and clinical trials.
“Just knowing what the cancer genes are, that’s important because now we can develop a cancer panel for screening” Dr Li Ding, one of the project’s major authors and associate professor of medicine and director of computational biology in oncology at Washington University, told The Independent.
Screening for the BRCA genes already takes place and can be used to help women choose the best treatment options.
In 2013 actress Angelina Jolie opted for a preventative double mastectomy after finding out she carried a mutation that meant she stood an 87 per cent chance of developing breast cancer.
“All those are important breakthroughs, but the most important thing we get is knowing what to do next,” Dr Li added.
With this in-depth understanding, treatment can be guided by the similarities in different cancer types, such as tumours of the cells lining the lung, bladder and head which had been previously been treated as separate diseases.
“Studying their molecular features, we now know such cancers are closely related,” said Dr Li. “Cancers originating in, for example, cells that line various organs are similarly closely related, regardless of their location.”
The project, launched in 2005, has reported its findings in a series of 27 papers, eight of which are published in the journal Cell today, signalling a new chapter in our understanding.
Insights about how one type of cancer relates to another form of the disease can have real clinical implications,” said Dr Josh Stuart, professor of biomolecular engineering at University of California Santa Cruz and one of the major contributors to the molecular analysis strand of the project.
“In some cases, we can borrow clinical practices from better-known diseases and apply them to cancers for which treatment options are less well defined.
“The milestone we hit with this paper is finally being able to stand back and look at the big picture.”
Independent researchers said the work opened up “new possibilities” but should be tested on patients.
“By revealing the molecular groups that cancers tend to fall into, this research opens up new possibilities for patients who would traditionally be treated based on where in the body their cancer is,” said Dr Justine Alford from Cancer Research UK.
“Identifying patients most likely to benefit from a particular treatment could also help improve clinical trials.
“The real test now will be to put this knowledge into practice and find out if this way of treating patients helps save more lives.”
The Independent
More about: cancer

























-1745485667.jpg&h=190&w=280&zc=1&q=100)